|
Do You Snore Loudly When You Sleep and Still Feel Tired in the Morning? If this describes you, then you may be experiencing sleep apnea. People with sleep apnea have a stoppage of their breathing for up to 30 seconds, perhaps hundreds of times during the night. There are two types - central sleep apnea (10% of cases) and obstructive sleep apnea or OSA (90%). Central sleep apnea is a rare brain problem and the muscles you breathe with do not receive the proper brain signals to make you breathe. OSA is caused by collapse and obstruction of your airway by the tongue, uvula, fatty tissue in the throat or relaxed throat muscles. If you have a sleep partner, he or she will be the first to discover this by the pauses in your breathing. In children, large tonsils and adenoids are problematic. To assess OSA severity and plan for treatment, a sleep study and physical exam are necessary. Aside from affecting quality of life, long-standing OSA can lead to heart disease by lowering your blood oxygen level, raising blood pressure, and altering heart rate thereby putting extra stress on your heart. Heart attack (3-fold increase), heart failure (2-fold increase), heart rhythm changes (e.g., atrial fibrillation) and sudden death are associated with OSA, and daytime drowsiness can lead to accidents. There is a 2-fold increase in all-cause mortality. Obesity (Body Mass Index over 35) is a frequent cofactor. After a careful physician exam, the STOP-BANG questionnaire1 provides confirming evidence. Next, a home sleep study or overnight polysomnography at a sleep laboratory showing 5-15 or more obstructive events per hour confirms the diagnosis. When the diagnosis is made, continuous positive airway pressure (CPAP) by mask is the first-line form of therapy.
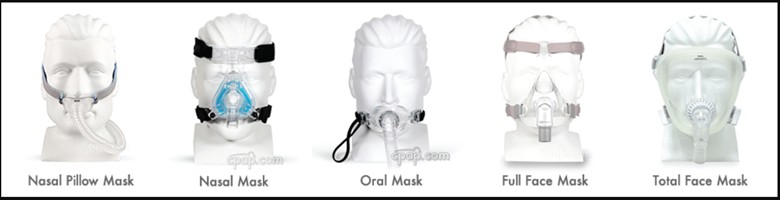
Respiratory Therapy Tip- If you are currently using CPAP or BiPAP therapy it is important to have your equipment checked to ensure it is set to your current pressure needs and air intake filters are clean. The mask should be cleaned at least weekly. Mask and hose should be replaced every 6 months or as needed. Many options are available for the mask so don’t give up if your first mask isn’t working for you!
Medical Tip from Dr. Charles Driscoll, VASSAR Surgeon General and Bruce Myer, VASSAR Past-President and Respiratory Therapist ———————————————————— References:
|